Birmingham research paves the way for new anti-fibrotic therapy for glaucoma
Scientists at the University of Birmingham have shown that a novel low molecular weight dextran-sulphate, ILB® could play a key role in treating open angle glaucoma (OAG), a neurodegenerative disease that affects over 70 million people worldwide and causes irreversible blindness.
OAG develops slowly over many years. Excessive matrix deposition (fibrosis) within the eye’s main fluid drainage site can lead to increased intraocular pressure (IOP), resulting in damage to the optic nerve.1
The research, reported in npj Regenerative Medicine, has shown that that ILB can normalise matrix deposition inside the eye and lower IOP in a pre-clinical model used to mimic these aspects of human glaucoma, paving the way for new anti-fibrotic therapies to be developed for the disease.
OAG is a complex disease and it has proved difficult to develop effective therapeutics to target the biochemical pathways involved. Existing therapies mainly work by reducing fluid production in the eye, not the underlying causes, and even the newer therapies have shown limited success in the clinic.2
The Birmingham scientists focussed on an inflammatory pathway that is common to several diseases, and involves Transforming Growth Factor β (TGFβ), a signalling molecule that communicates between cells and orchestrates both inflammation and fibrosis. TGFβ’s role in OAG is well known, with patients demonstrating higher levels in their aqueous humour and laboratory studies showing that artificially increasing TGFβ within the eye can lead to fibrosis3,4.
The scientists found that ILB has multimodal actions across many genes that resolve inflammatory and fibrotic cellular processes. When they progressed their work into a pre-clinical experimental model of glaucoma, they found that daily subcutaneous injections of ILB significantly (p<0.01) reduced extracellular matrix levels within the eye’s main drainage site, normalised the eye’s pressure and prevented degeneration of retinal neurons. The research was conducted by Dr Lisa Hill, from the Institute of Clinical Sciences, and Dr Hannah Botfield, from the Institute of Inflammation and Ageing. They commented: “We are truly excited by these results, which show a way forward for a glaucoma treatment that can reverse the fibrotic process that causes the disease.”
Clinicians working in ophthalmology generally prefer local over systemically delivered therapeutics, as it is a safer route of administration that is more acceptable to patients.
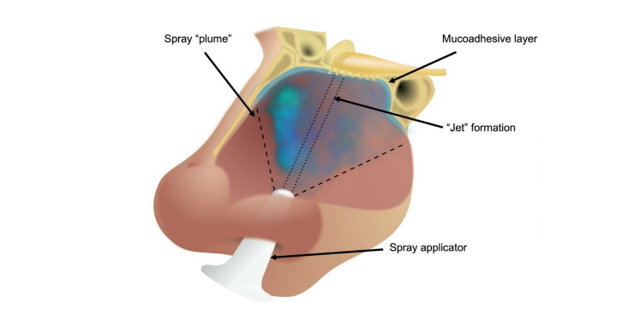
Dr Hill is leading a project to formulate a topical alternative that will avoid the need for injection. She is working closely on this with Mr Imran Masood, a consultant ophthalmic surgeon at Sandwell and West Birmingham NHS Trust and Professor Liam Grover, a biomaterials expert from the ITM-based Healthcare Technologies Institute, to assess the use of a novel shear thinning fluid gel for the resolution of glaucoma.
The shear thinning fluid gel was developed for use as eye drops that are retained for an extended period of time following administration, and patents have been filed for its use both alone, and in combination with other therapeutics.5 Previous studies have shown the fluid gel reduces corneal scarring when applied topically, and it is an effective carrier molecule for other therapeutics.6
ENDS
ILB® resolves inflammatory scarring and promotes functional tissue repair has been published in NPJ Regen Med. DOI: 10.1038/s41536-020-00110-2
For further media information contact Ruth Ashton, Reputation and Communications Development Manager, University of Birmingham Enterprise, email: r.c.ashton@bham.ac.uk
For further information about the fluid gel patent, contact Helen Dunster, Business Development Manager, University of Birmingham Enterprise, email: H.Dunster@bham.ac.uk
About ILB®
ILB® is a unique and distinct LMW-DS formulation whose structure, formulation, synthesis and relevance to fibrotic diseases like glaucoma has been described in detail previously in two published patents (WO 2016/076780 and WO 2018/212708). For this study, ILB® (batch number 3045586) was provided by Tikomed AB.
The study also benchmarked ILB® against an approved anti-fibrotic drug, pirfenidone, in cultured human cells, where it showed a unique anti-inflammatory response.
About University of Birmingham Enterprise
University of Birmingham Enterprise helps researchers turn their ideas into new services, products and enterprises that meet real-world needs. We also support innovators and entrepreneurs with mentoring, advice, and training and manage the University’s Academic Consultancy Service.
References
- Tektas, O. Y. & Lutjen-Drecoll, E. Structural changes of the trabecular meshwork in different kinds of glaucoma. Experimental Eye Research, 88(4), 769-75 (2009).
- Friedman, S. L., Sheppard, D., Duffield, J. S. & Violette, S. Therapy for fibrotic diseases: Nearing the starting line. Science Translational Medicine 5(167), 167sr1-sr1 (2013).
- Fuchshofer, R. & Tamm, E. R. The role of TGF-beta in the pathogenesis of primary open-angle glaucoma. Cell and Tissue Research, 347(1), 279-90 (2012).
- Kim, K. S., Lee, B. H. & Kim, I. S. The measurement of fibronectin concentrations in human aqueous humor. Korean Journal of Ophthalmology, 6(1), 1-5 (1992).
- Patent numbers: WO/2020/115510; WO/2020/115508; GB2008919.9
- Hill et al. Sustained release of decorin to the surface of the eye enables scarless corneal regeneration. npj Regenerative Medicine. 3, 1-12 (2018).